NC State student with cystic fibrosis does scientific research seeking to cure ailments like hers
Published 12:10 am Sunday, March 5, 2023
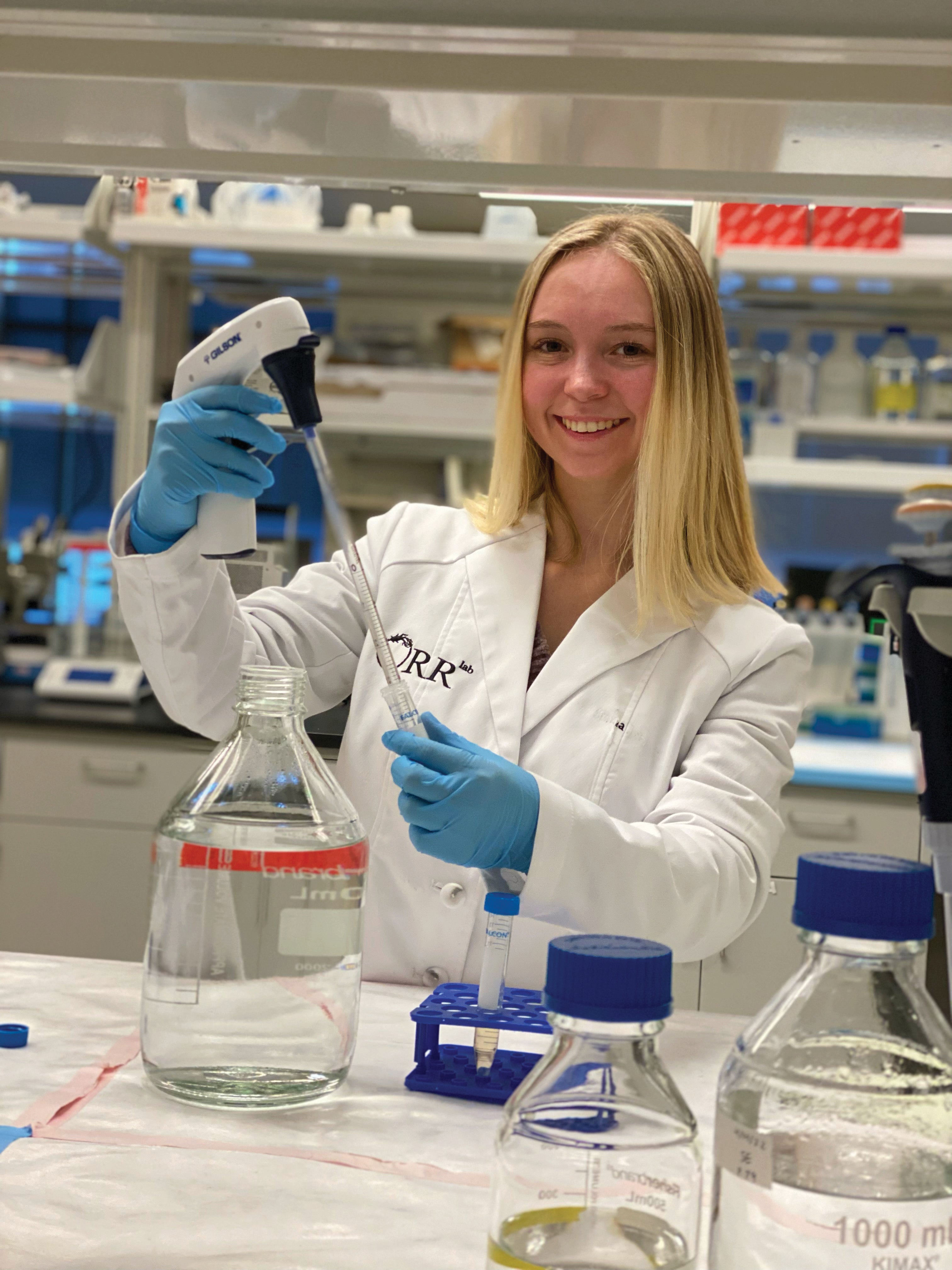
- Grace Hodge was diagnosed with cystic fibrosis when she was 3, but that has inspired her to work toward helping cure all kinds of diseases. Submitted photo
SALISBURY — Grace Hodge wants to help as many people as she can since being diagnosed with cystic fibrosis when she was 3. She’s also doing everything in her power to make sure anyone who is dealing with a disease like her doesn’t become defined by their diagnosis.
“Your life is not sickness, it’s not despair. You have joy and you have light and that’s something that you need to remember,” said the Cleveland resident who is now at N.C. State University.
Cystic fibrosis is a genetic disease that causes an increased amount of mucus in the lungs and pancreas. Symptoms include malnutrition, poor growth, frequent respiratory infections, breathing problems and chronic lung disease. Normally, Grace’s doctors would have realized she had the disorder before she was 3, but North Carolina didn’t have mandatory newborn screenings at the time she was born.
Grace’s mom started to notice things were wrong as she grew. She took her to the doctor and and made them test Grace for a bacteria in her stool called pseudomonas. That’s when they found out she had it. “My mom is the one who figured it out and not any doctors,” Grace said.
She was hospitalized immediately afterwards for treatment to make up for the time before she was diagnosed. She got the necessary medical equipment and medication to help with the mucus. Growing up, her symptoms weren’t as severe, but she still had to make two-week trips to the hospital twice a year.
“Being a child and in school, you kind of stress about those things, but I would sit in my hospital room and do my schoolwork and still get my treatments,” Grace said.
Usually as people get older, cystic fibrosis gets worse, but Grace’s hospital visits decreased to the point where she hasn’t had a serious problem in several years. In 2019, genetic modulator treatment was introduced to deal with cystic fibrosis and it has done wonders for her overall health.
“My two mutations, I have a protein channel, but my protein is misfolded so it can’t get through to the right channel,” Grace said.
Genetic modulator treatment got the protein folded correctly and cut down on her symptoms significantly, “which was amazing at that time and it was something brand new that they never had much success doing that before,” she said.
Now 20 and majoring in biological sciences, she hasn’t been seriously hospitalized since 2016. She said her current doctors are “amazed at my progress.”
Still, Grace has a routine that requires her to do breathing treatments twice a day, wear a lifejacket-type machine that pulsates air to shake the mucus out of her lungs and take daily medication. By now, she’s gotten the hang of it and is feeling better than ever.
“There’s very little mucus production, I’m able to walk to class and be fine, I’m able to play sports if I chose to. There’s not many things now that hinder my day-to-day activities,” Grace said.
Originally, she had dreams of becoming a doctor and working as a pediatric pulmonologist, which is the kind of specialist she sees for CF, but when she realized there wouldn’t be a cure in the near future, she decided to start working in genetic biology.
“That’s just what I find most fascinating,” Grace said.
At N.C. State, her first year of college was during COVID, so she didn’t get hands-on experience she needed. At such a large school, she was not able to get into any of the labs for research.
Luckily, her mother works at the W.G. “Bill” Hefner VA Medical Center in Salisbury, where she learned about the VA South Central Appalachian Network for Research Development (VA SCAN-RD) program. It focuses on “limited access to research opportunities for underserved, minority and rural veterans.”
After she was accepted, she finally got do the kind of work she had been wanting to do for as long as she could remember. “That was able to give me enough boost that I felt like I needed to really know that this is what I wanted to go in to,” Grace said.
Her mentor, Dr. Miranda Orr, works at the Wake Forest University School of Medicine, where research for the VA SCAN-RD takes place. Orr is impressed with the work Grace is doing and also with her as a person.
“You would not even know she has this disease that she is dealing with every day,” Orr said. “You would never know. She is just so optimistic, so cheerful. She’s just a really remarkable young lady.”
Last summer, Grace went to Wake Forest a few times a week to be a part of Orr’s research and was able to learn basic laboratory techniques, how to measure correct amounts, the ethics involved in research, communication, collaboration and analysis of results.
Grace is happy to have someone like Orr to guide her. “She’s been the most in-depth mentor, lab technician, lab leader that I’ve ever had,” Grace said.
“It’s incredibly rewarding to provide research opportunities to very young, curious adults hoping to get them more engaged in science and think about all the different career paths,” Orr said.
Grace will be in the VA SCAN-RD again this summer. This time, she’ll have more freedom with her work. Grace wants to get into gene therapy and help cure diseases, even if it’s not CF. “I’m more interested in to being able to really conduct my own research and hopefully get a poster or a paper, my name out there somewhere,” Grace said.
She has had plenty of emotional and medical support, but doesn’t know yet what she wants to focus on after she graduates. She does have an idea. “I want to be able to go somewhere that can help fuel progress,” she said.
As her symptoms remain manageable, Grace is making the most of her potential and not letting CF shape who she is.
“I think that the most important thing that you can do when having a chronic, progressive disease is hope. … I think that it’s important to keep who you are inside and yes, have CF be a part of you, but it is not who you are,” Grace said.





